Healthcare changemakers
Shaping the future of healthcare
Feby Abraham, Chief Strategy Officer of Memorial Hermann Health System, is shaping the future of access, experience, outcomes, and engagement.
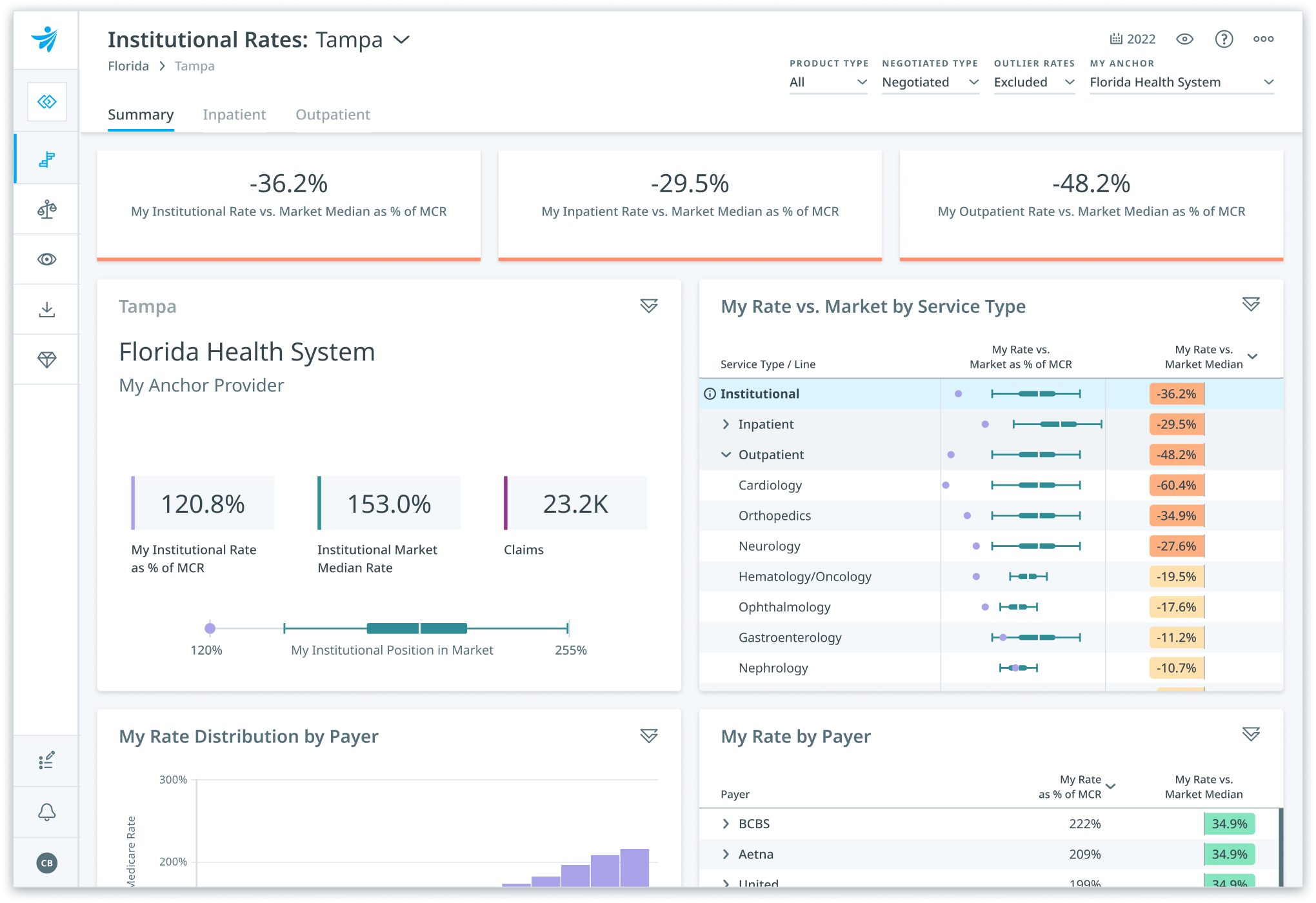
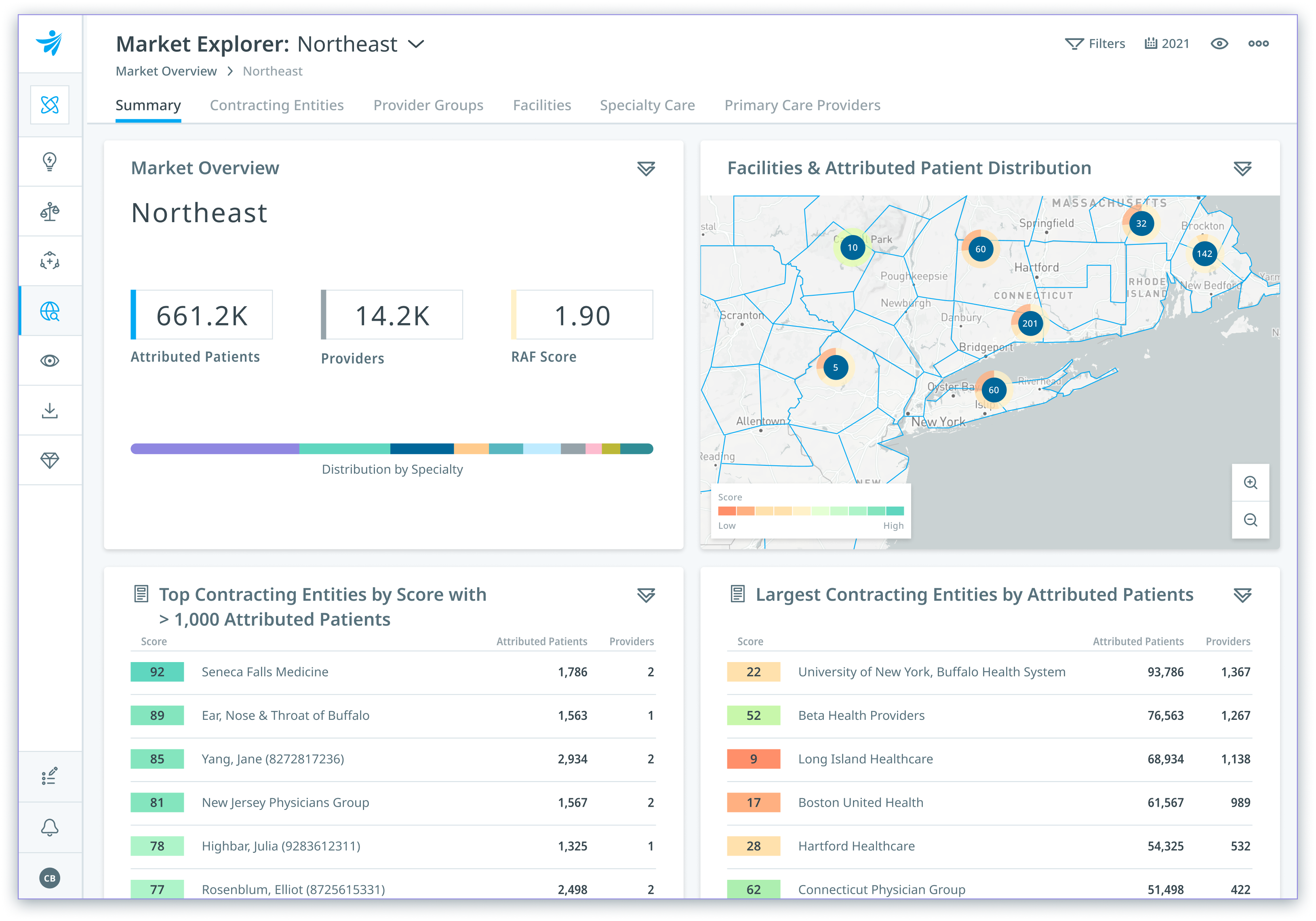
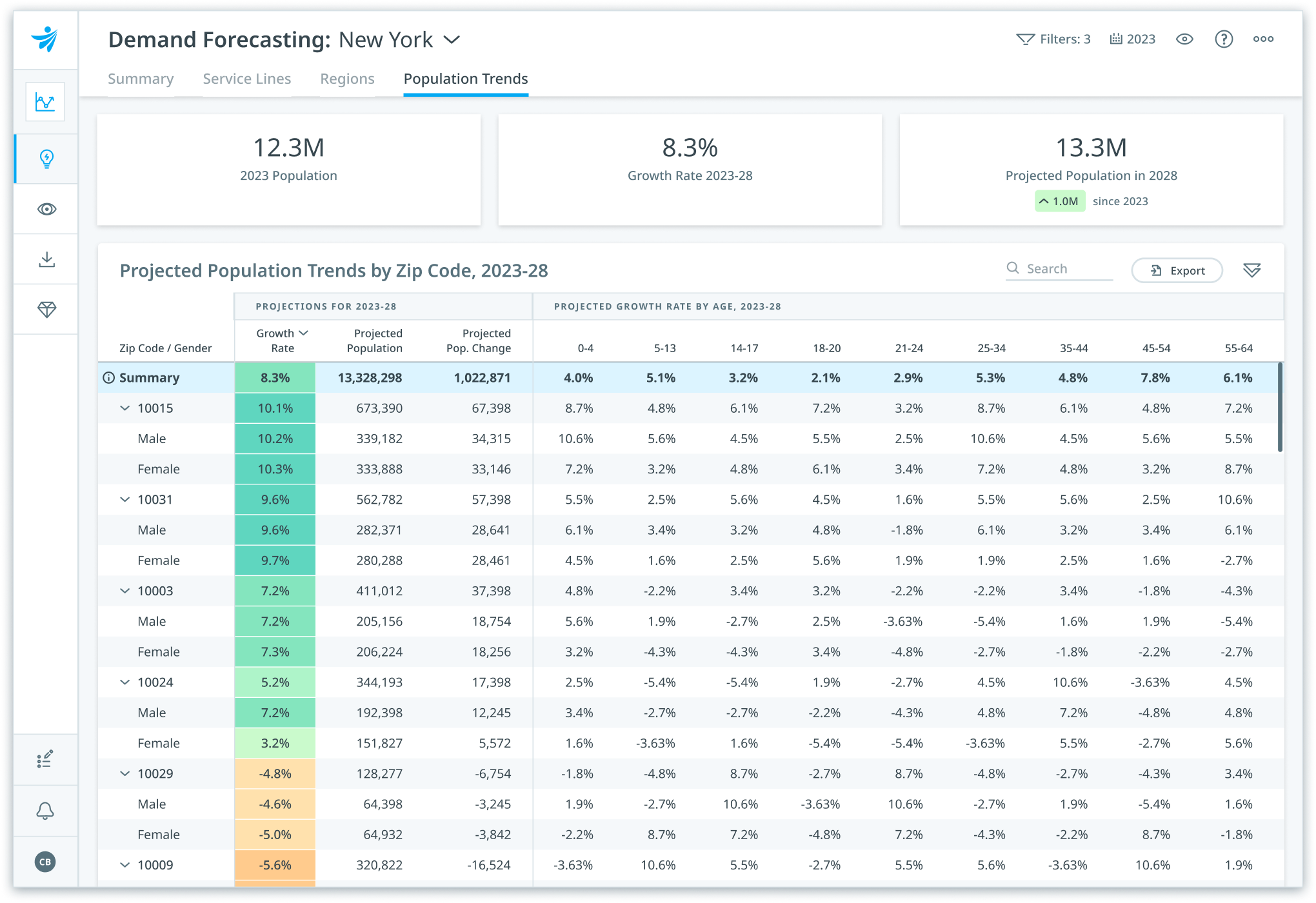
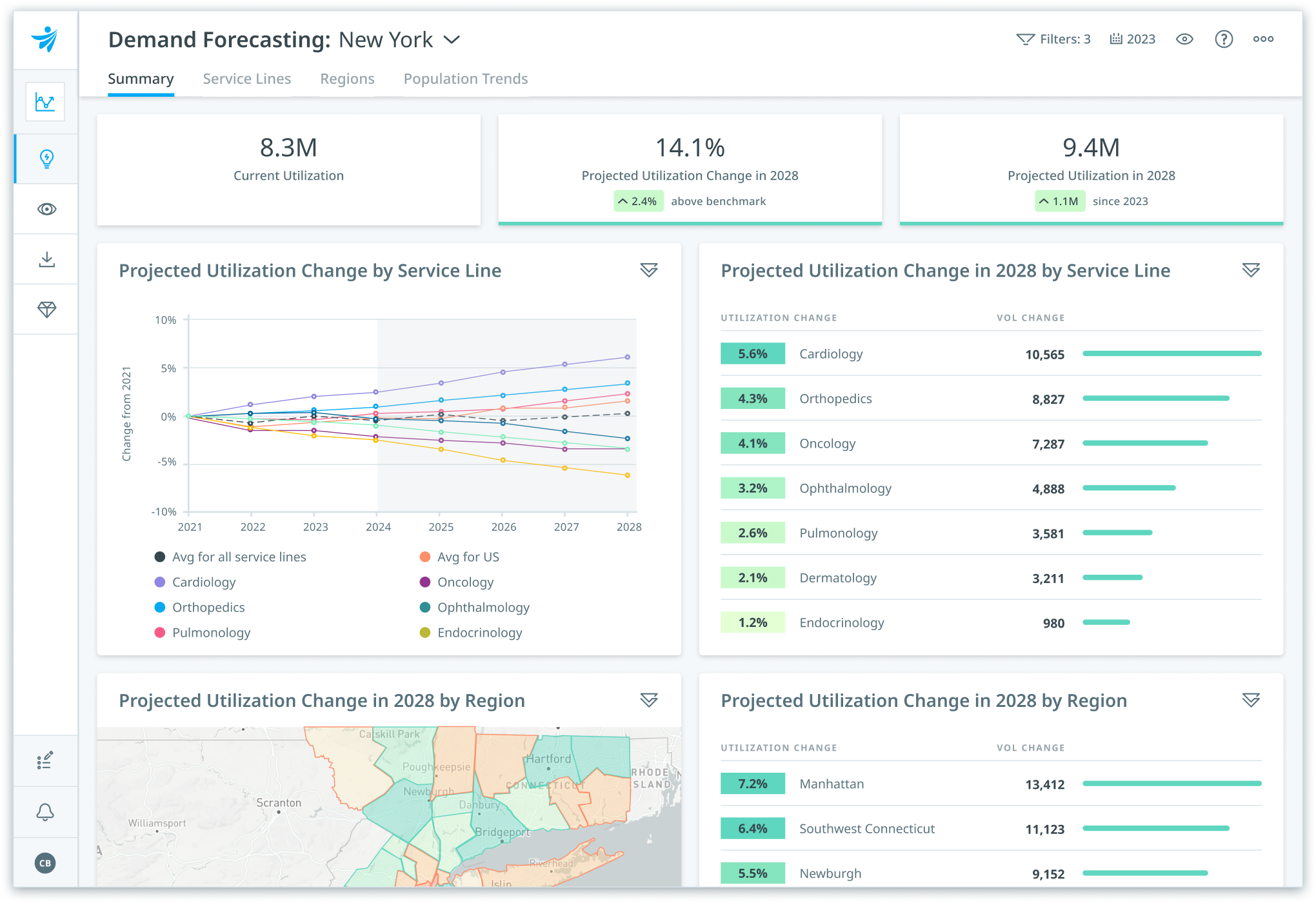
Get insights into market dynamics, patient journeys, price transparency, and future healthcare demand to lead in your market.


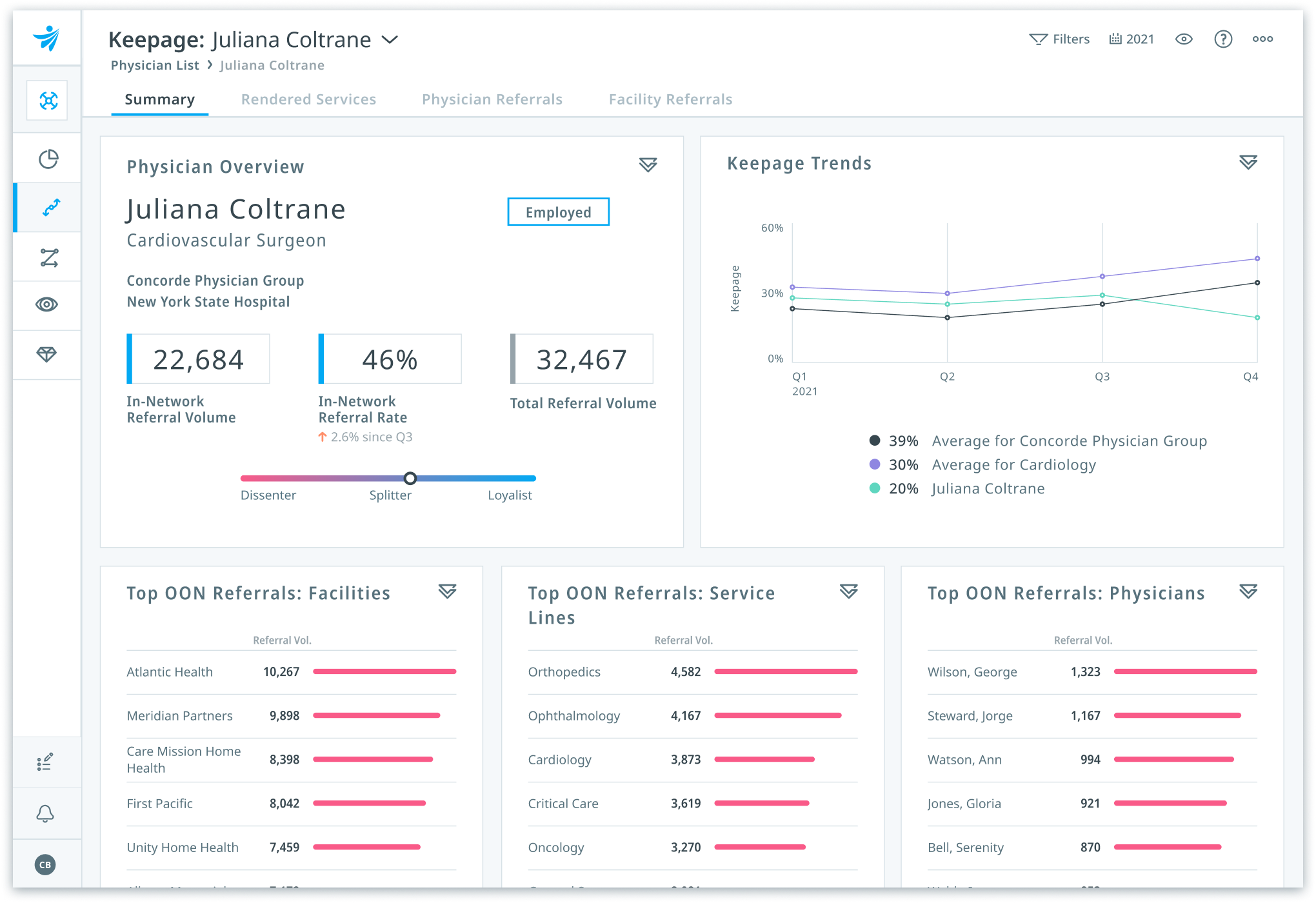
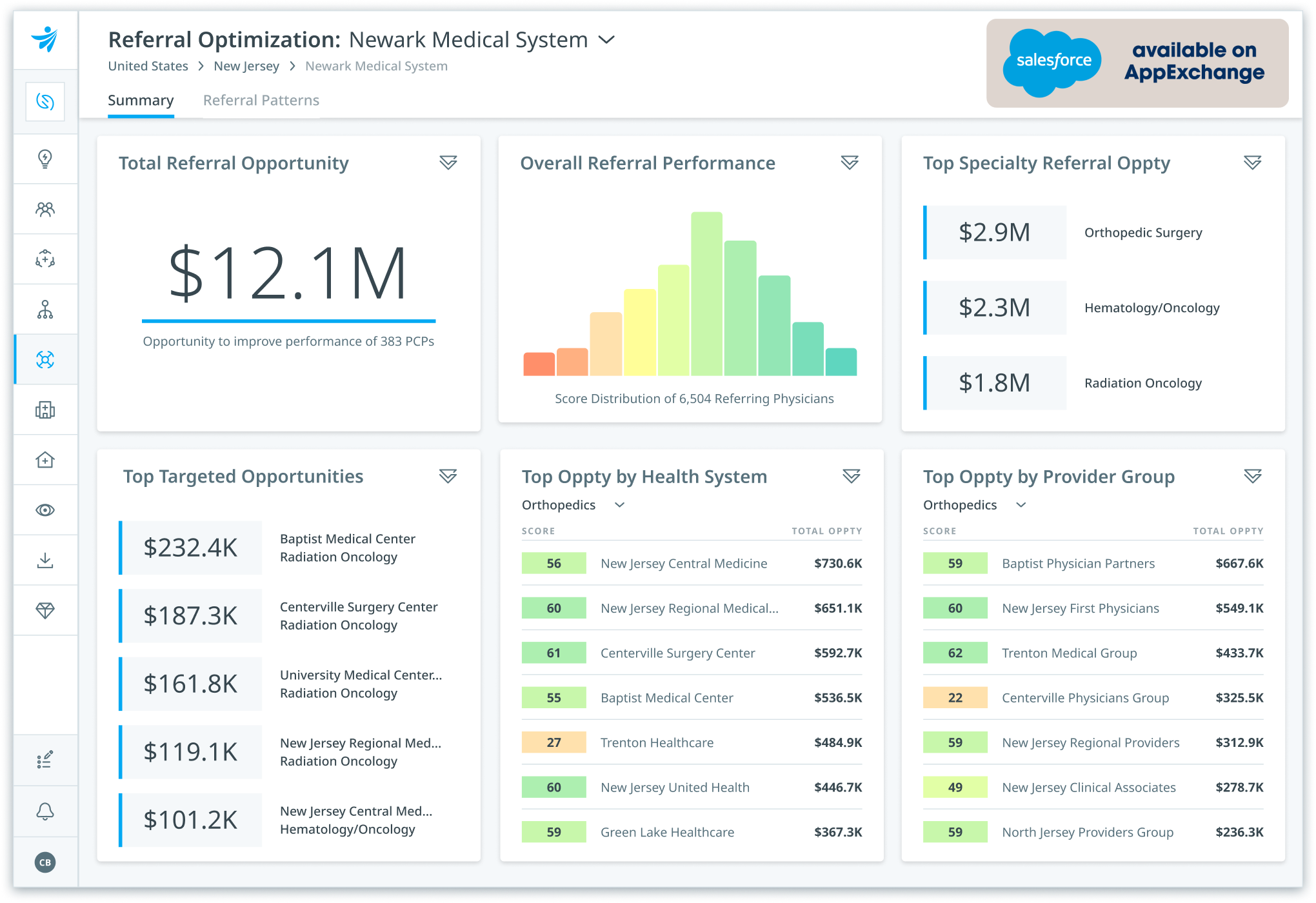
“Clarify has given us the most granular insights across our entire market – we can see what physicians are doing, where they’re going, who they’re referring to, and how their patterns change by procedure.”
David Stephens
Vice President, Network Strategy and Business Development
Hackensack Meridian Health
Save while supporting long-term growth
As healthcare providers maintain a dual focus on growth and cost management, business leaders are identifying areas to generate cost savings and support their long-term growth.
Drive strategic growth
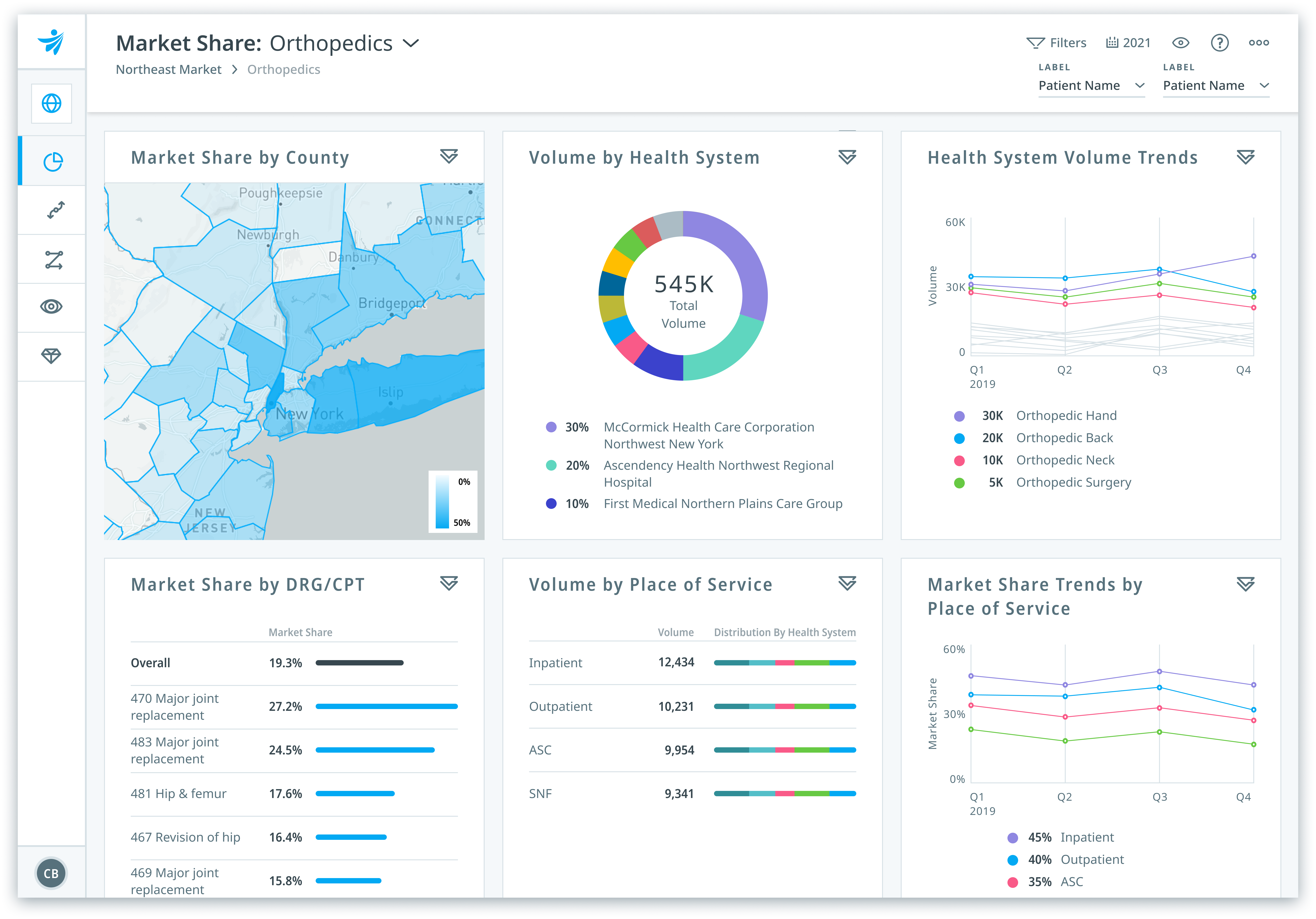
Grow patient volume

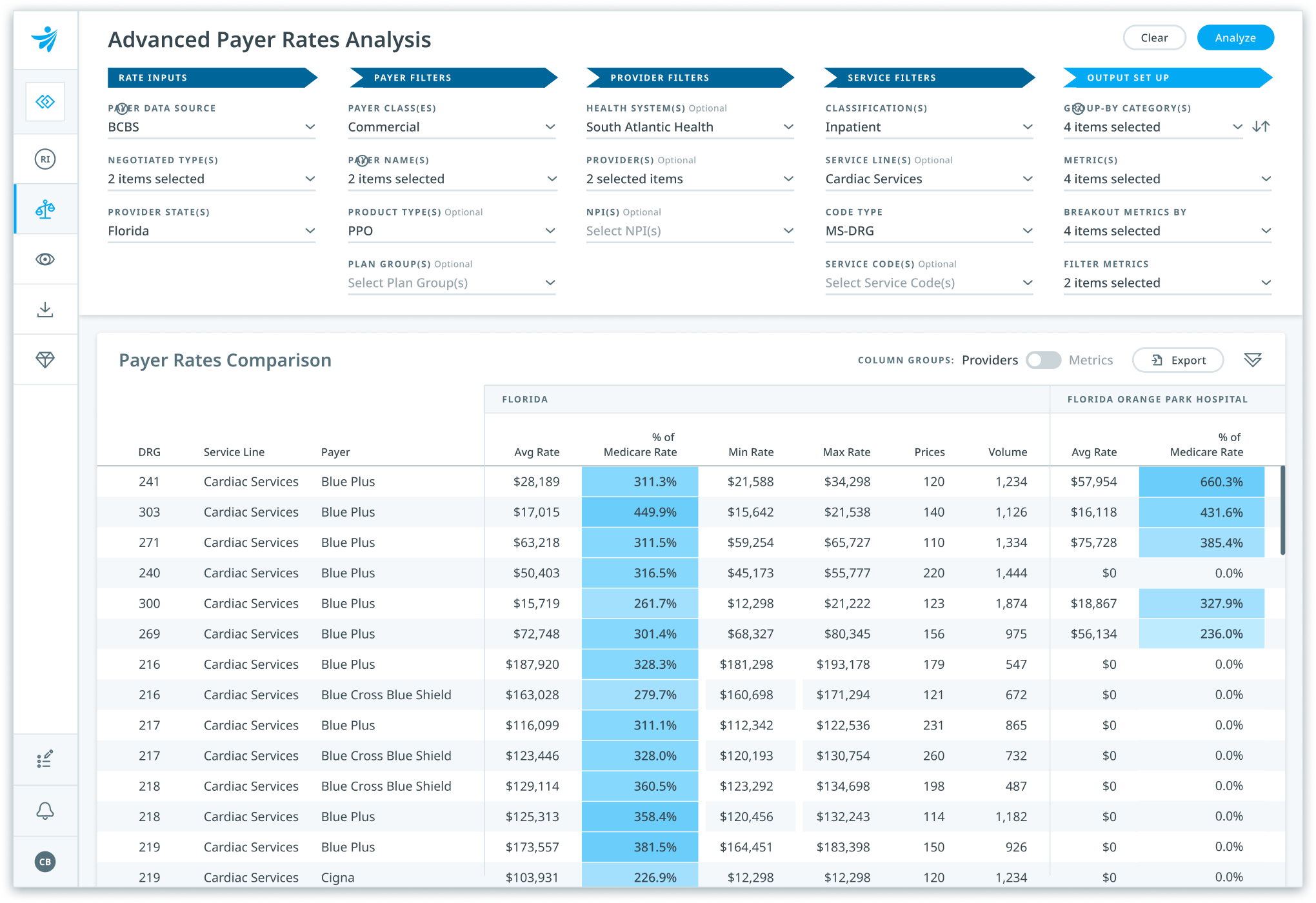
Strengthen rate negotiations
Drive greater value
Forecast healthcare demand
$50M
opportunity to grow oncology business
$3.5M
care delivery savings
Big Data Simplified: Clarify’s platform gives us a lens into how we perform in comparison to other nationally recognized organizations.”
Clarify is solving the issue of identifying physicians with the greatest amounts of quality and efficiency in a market to utilize in development discussions.”
Getting referral analytics in the hands of our operations team and our physicians was critical to effectively establish centralized service coordination. Clarify’s partnership allowed us to have transparency into the data, engage with the analytics, arrive at meaningful insights, and develop the right processes.”
Insights for Providers
Insights for Providers
Insights for Providers
Insights for Providers
Insights for Payers
Insights for Providers
Insights for Providers
Video
Healthcare Analytics
Healthcare Analytics
Hospital Growth Strategy
Hospital Growth Strategy
Hospital Growth Strategy
Healthcare Analytics
Healthcare Analytics
Healthcare Analytics
Insights for Payers
Insights for Payers
Value-Based Care (VBC)
Insights for Payers
Insights for Payers
Healthcare Price Transparency
Insights for Payers
Video
Healthcare Price Transparency
Insights for Providers
Video
Insights for Providers
Insights for Providers
Video
Video
Video

Accelerate transformation, drive growth, and adopt innovative payment models confidently with the industry’s most trusted healthcare analytics platform, mapping over 300 million real-world patient journeys with machine-learning precision.